The human body possesses an extraordinary capacity for self-healing, a phenomenon that has long fascinated both scientists and clinicians. Among the most intriguing manifestations of this innate ability is the placebo effect – the well-documented phenomenon where patients experience real physiological improvements after receiving inactive treatments they believe to be therapeutic. Now, emerging research suggests we may be able to harness these mind-body mechanisms to activate immune responses without pharmaceutical intervention.
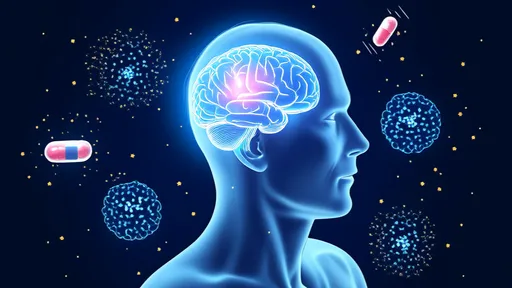
For decades, the placebo effect was dismissed as mere psychological trickery. However, modern neuroscience reveals a far more complex picture. When a person expects healing, their brain releases a cocktail of neurotransmitters and hormones that can directly influence immune function. Dopamine, endogenous opioids, and cannabinoids all play roles in this psychoneuroimmunological cascade. Recent studies using advanced brain imaging show that placebo responses activate the same neural pathways as actual medications in conditions ranging from depression to Parkinson's disease.
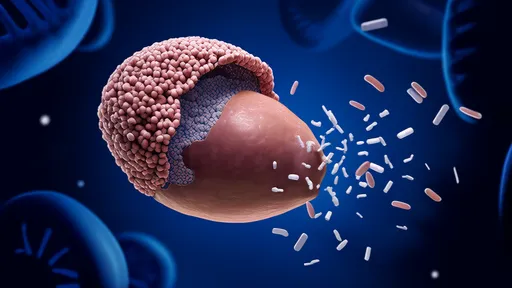
The implications for immunity are particularly exciting. In controlled trials, researchers have observed measurable changes in immune markers when participants believed they were receiving immune-boosting treatments. One landmark study demonstrated that volunteers who thought they were taking an immune-stimulating drug showed increased natural killer cell activity – even though they received only saline injections. These findings challenge our traditional separation between mind and body, suggesting that psychological states can directly shape physiological defenses.
How might this work in practical terms? Several research teams are exploring non-pharmacological approaches to trigger these beneficial placebo-like effects. Conditioned responses appear particularly powerful – when the body learns to associate certain rituals or environments with immune activation. In one innovative experiment, patients who had previously taken real immunosuppressant drugs maintained therapeutic benefits when switched to placebos, provided the administration context remained identical. This demonstrates how environmental cues can become biological triggers.
The ethical dimensions of this research require careful consideration. While placebo effects offer exciting possibilities for reducing medication dependence, clinicians must balance this with transparent patient communication. New protocols are being developed that employ "open-label placebos" – where patients knowingly take inert substances while understanding the science behind mind-body healing. Surprisingly, these approaches often work nearly as well as traditional concealed placebos, especially when combined with explanations of the body's innate healing capacities.
Looking ahead, researchers are investigating how to optimize these effects. Meditation, visualization techniques, and even certain types of psychotherapy may help individuals cultivate mental states conducive to immune enhancement. Early evidence suggests that people with stronger mind-body awareness and those who score high on measures of suggestibility tend to experience more pronounced placebo responses. This doesn't imply the effects are "all in the head" – rather, it points to individual differences in psychophysiological connectivity that we're only beginning to understand.
As this field advances, we may see the development of "placebo-plus" protocols that combine traditional healing rituals with modern scientific understanding. Imagine clinics where carefully designed environmental cues, practitioner interactions, and cognitive exercises work synergistically to mobilize the body's defenses. Such approaches wouldn't replace conventional medicine but could complement it, potentially reducing side effects and healthcare costs while empowering patients.
The implications extend beyond clinical settings. If we can better understand how expectations and beliefs influence immunity, we might apply these principles to daily life. Simple practices like maintaining positive health expectations or creating personal healing rituals could have measurable impacts on wellbeing. While more research is needed, the growing evidence suggests that our minds may be the most underutilized resource in healthcare – not as substitutes for medicine, but as powerful allies in the healing process.
This exploration of placebo mechanisms represents more than just scientific curiosity. It reflects a paradigm shift in how we conceptualize health and treatment. By mapping the intricate pathways connecting mental states to immune function, we're rediscovering ancient wisdom about the unity of mind and body – now with rigorous empirical support. The future may hold ways to consciously access these innate healing capacities, potentially transforming how we approach wellness and disease prevention.

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025