The Illusion of Pain: Rethinking Phantom Limb Pain Through the Brain's Deception
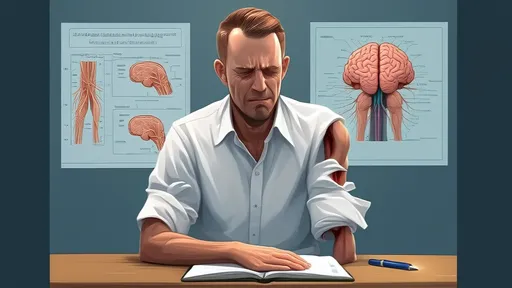
For centuries, phantom limb pain has baffled both patients and physicians. The sensation of pain or discomfort in a limb that no longer exists defies conventional logic, yet it remains a harrowing reality for many amputees. Recent advances in neuroscience, however, are challenging our understanding of this phenomenon—suggesting that pain, in many cases, is not a direct response to physical injury but rather a construct of the brain. This revelation is opening doors to innovative treatments that target the mind rather than the missing limb.
The concept of pain as a "lie" fabricated by the brain may sound counterintuitive, but mounting evidence supports this idea. When an individual loses a limb, the brain's neural map of the body doesn’t immediately update. The regions that once processed signals from the missing limb remain active, sometimes firing erratically. These misfires can generate sensations—tingling, itching, or even excruciating pain—that feel as real as any physical stimulus. In essence, the brain is trapped in an outdated perception of the body, unable to reconcile the absence of the limb with its ingrained expectations.
Traditional approaches to phantom limb pain have often focused on the stump or peripheral nerves, with treatments ranging from medications to nerve blocks. While these methods provide relief for some, they frequently fall short, leaving patients in persistent agony. The emerging paradigm shift centers on the brain’s plasticity—its ability to rewire itself. Therapies like mirror therapy, where patients use visual feedback to "move" their missing limb, exploit this plasticity. By tricking the brain into perceiving movement where there is none, the neural confusion causing the pain can gradually dissolve.
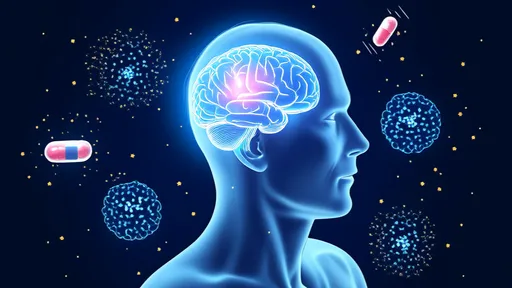
Another groundbreaking avenue is virtual reality (VR). In immersive VR environments, amputees can interact with a digital representation of their lost limb, performing tasks that would have been impossible in reality. Studies have shown that this visual and motor reinforcement can recalibrate the brain’s distorted body map, reducing or even eliminating phantom pain. The success of VR therapy underscores a critical insight: pain is not just a symptom but a maladaptive narrative the brain clings to, one that can be rewritten.
Perhaps the most radical development comes from the field of neurofeedback. By allowing patients to observe their own brain activity in real time, they can learn to modulate the regions responsible for phantom pain. This self-regulation, akin to training a muscle, empowers individuals to dismantle their pain from within. Early trials have reported astonishing results, with some participants experiencing lasting relief after just a few sessions. The implications are profound—if pain is a story the brain tells, then patients can become the authors of their own healing.
Yet, skepticism persists. Critics argue that these mind-centric approaches overlook the complexity of pain, which often involves a tangled web of physiological, psychological, and social factors. Moreover, not all patients respond equally to these therapies, highlighting the need for personalized treatment plans. Nevertheless, the growing body of research supporting the brain’s role in phantom pain is impossible to ignore. It challenges us to reconsider not just how we treat pain, but how we understand it.
For amputees like David, who endured years of relentless phantom pain after losing his arm in an accident, these innovations have been life-changing. After failing with conventional treatments, he turned to mirror therapy and later VR. "It felt like my brain was finally catching up to reality," he says. "The pain didn’t vanish overnight, but it lost its grip on me." Stories like David’s are fueling optimism among researchers, who believe that the key to conquering phantom pain lies not in the body’s periphery, but in the mind’s remarkable capacity for deception—and, ultimately, for healing.
As science continues to unravel the mysteries of phantom limb pain, one thing becomes clear: pain is far more than a sensory signal. It is a narrative, shaped by the brain’s expectations, memories, and even its mistakes. By confronting this narrative head-on, we may finally unlock the door to lasting relief for millions who suffer in silence.

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025